|
The confidence that there will always be facilities and professionals to care for us is no longer realistic. I’ve covered the systemic problems of U.S. healthcare for over a decade, and as a result I’ve attracted numerous healthcare professionals as correspondents. I’ve been corresponding with some for almost 15 years, and this correspondence has given me a sobering education in the realities of our fully financialized (and thus hollowed-out) healthcare system. I’ve shared many of the professionals’ insights over the years, for example: Can “Sickcare” Survive the Pandemic? (April 14, 2020) Like the rest of the financialization machine, sickcare was never sustainable. The hollowing out of financialization has been accelerating for over a decade. In effect, there are two tiers of healthcare: the “sickcare” system managed by profiteering, predatory, parasitic corporations and their non-healthcare managers/shareholders who are seeking the $30 million payday, the $300 million payday or the $3 billion payday. |
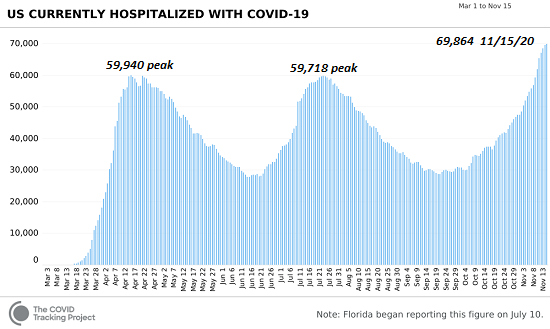
Covid hospitalized |
| The second tier is composed of the overworked, over-regulated healthcare professionals trying their best to provide care within the hollowed out, unaffordable dysfunctional, unsustainable “sickcare” system of rapacious cartels, compliance managers, debt deals, lobbyists, unsafe medications passed off as “safe,” off-patent medications brought back under patent protection via pathetically transparent formula tweaks, billions of dollars of pharmaceutical adverts directed at patients, a practice that was illegal a generation ago, and so on in an endless profusion of skims, scams, rackets and corruption.
Needless to say, operating in a system that optimizes greed, profiteering and corruption and views healthcare as a profit-maximizing venture is difficult for everyone but the sociopaths at the top raking in millions. Those in the lower tier trying to deliver care are finding a system shredded by cost-cutting (i.e. profit-maximization), stripped of supplies and burdened by counterproductive standards of care and punitive compliance regulations. The demands to treat the soaring caseload of Covid patients are pushing the system toward breakdown. As the chart of Covid hospitalizations shows, current hospitalizations are already 10,000 above previous peaks (70,000 compared to 60,000) and are estimated to reach 100,000 within a few weeks. A significant percentage of health care personnel (HCP) contract Covid, and 4% of those who are hospitalized have died: Analysis of COVID-19 hospitalization data from 13 sites indicated that 6% of adults hospitalized with COVID-19 were HCP. In addition to the very real risks to their own health, many healthcare professionals have parents, children or grandchildren to care for at home, and so the risks they face at work impact their families and that influences their life decisions. How much risk and stress can one absorb before it’s no longer worth it or it’s no longer possible to force yourself to endure another exhausting shift? |
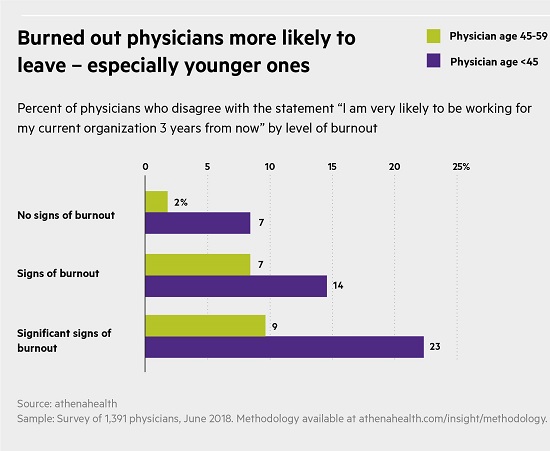
Burnout physicians |
| As shifts become longer, burnout becomes a real threat. Even before covid, burned out physicians were leaving, as this chart reveals:
Doctors Are Calling It Quits Under Stress of the Pandemic (NYT.com) Thousands of medical practices are closing, as doctors and nurses decide to retire early or shift to less intense jobs. Burnout Nation (May 14, 2019) ‘I cry before work’: US essential workers burned out amid pandemic Essential workers reported stress caused by increased workloads, understaffing, fears over Covid and struggles in enforcing social distancing.
Most Americans don’t seem to realize that once the Covid wards are full and the hospitals are understaffed, there won’t be anyone left to provide care. As occurred in Wuhan, China, patients will be turned away because there are no more beds in Covid wards, and not enough personnel to staff temporary facilities. Most people don’t seem to appreciate the pressure being placed on overworked healthcare professionals or the consequences of mass burnout. At some point, people have to protect their own health and families, just like everyone else. |
US healthcare, 1960-2010 |
| The confidence that there will always be facilities and professionals to care for us is no longer realistic. The U.S. healthcare system has been stripped of redundancy and buffers because neither served the almighty bottom-line. In effect, the system has been optimized to serve limited numbers of ICU and critical-care patients. There is no way to suddenly optimize this complex system for 100,000+ Covid patients and also care for the thousands of patients who are suffering from injuries or other critical conditions.
The exponential rise in cases will lead to an equivalent exponential rise in hospitalizations— an increase that may well exceed the capacity of the system. Beyond this tipping point, the system– like any system–breaks down and ceases to function. Lastly, it’s important to understand that demands for care will increase even if 100% populace eventually accepts a 100% effective vaccine (a dubious assumption for many reasons), as many of those recovering from Covid will require higher levels of care for months and possibly even years (Long Covid is poorly understood). Medical costs of discharged German COVID patients 50% above pre-admission levels Here are a handful of the dozens of posts I’ve written addressing systemic issues in healthcare: Healthcare “Reform”: the State and Plutocracy Stripmine the Middle Class (Again) (November 9, 2009) The Inevitable Collapse of the “Healthcare”/Sickcare System (November 12, 2009) Sickcare Will Bankrupt the Nation (March 21, 2011) the Healthcare System Is Completely Broken (March 27, 2017) |
The bankrupt U.S. healthcare system |
Full story here Are you the author? Previous post See more for Next post
Tags: Featured,newsletter